Rheumatic Fever in Children: The Complete Guide Parents Should Read
1.What Is Rheumatic Fever?
Rheumatic fever is a preventable inflammatory disease that most often affects children between ages 5 and 15. It occurs as a delayed immune response to a streptococcal infection (strep throat or scarlet fever) that wasn’t properly treated with antibiotics. Although rare in many developed countries, it remains an important childhood health concern in many parts of the world.
Instead of being contagious itself, rheumatic fever is an autoimmune reaction — the immune system mistakenly attacks the body’s own tissues, especially the heart, joints, skin, and sometimes the brain.
2.What Causes Rheumatic Fever?
The disease develops after infection with group A Streptococcus bacteria. These bacteria cause common illnesses like:
-
Strep throat
-
Scarlet fever
If these infections are left untreated or not fully treated with antibiotics, the child’s immune system can create antibodies that later attack healthy tissues in the body. This is what leads to rheumatic fever.
There is still no single test that explains exactly how this autoimmune response happens, but the result is inflammation throughout the body.
3.Who Is Most at Risk?
Rheumatic fever can affect anyone who has had a strep infection, but certain groups are more at risk:
-
Age 5–15: This is the most common age range.
-
Untreated strep throat: The biggest risk is not completing a full course of antibiotics.
-
Crowded living conditions: Schools, homes with many people, and places without easy access to medical care raise risk.
-
Repeated strep infections: Recurring infections heighten the risk of rheumatic fever.
Rheumatic fever is less common in children under age 3 and adults, and very rare in places where strep infections are quickly treated.
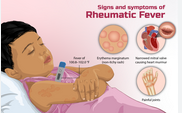
4.Signs & Symptoms to Watch For
Symptoms typically appear 2 to 4 weeks after a strep infection. They can vary widely from child to child, and some symptoms might appear mild or easy to miss.
Common Symptoms
-
Fever
-
Painful, swollen joints (knees, ankles, elbows, wrists) that may move from one joint to another
-
Small, painless nodules under the skin
-
Red rash with irregular edges
-
Chest pain or palpitations
-
Extreme fatigue or weakness
Neurological Signs
Some children develop Sydenham chorea, which includes:
-
Jerky, uncontrollable movements
-
Emotional outbursts (crying or laughing without cause)
Heart Symptoms
When the heart is inflamed (a condition called carditis), signs can include:
-
Rapid heartbeat
-
Shortness of breath
-
Chest discomfort
-
Heart murmurs detected by a doctor
5.How Is Rheumatic Fever Diagnosed?
Diagnosis is based on a child’s medical history, symptoms, physical examination, and tests. Doctors often use a set of criteria called the Jones criteria to confirm a diagnosis.
Typical Diagnostic Steps
-
Throat swab to check for strep bacteria
-
Blood tests to detect signs of past strep infection and inflammation
-
Heart tests, like an EKG or echocardiogram, to check heart function
-
Presence of symptoms like arthritis, rash, chorea, and fever helps confirm diagnosis.
6.Treatment Options
There is no cure for rheumatic fever once it develops, but treatments can manage symptoms, reduce inflammation, and prevent long-term damage.
1. Antibiotics
Antibiotics such as penicillin are used to kill any remaining strep bacteria and prevent recurrences. In many cases, a child might take antibiotics for several years — sometimes through age 21 — to prevent future episodes.
2. Anti-Inflammatory Medicines
Medications like aspirin or naproxen can reduce pain and inflammation. For more severe swelling, doctors may prescribe corticosteroids. Only give aspirin to children under medical advice, as it must be used carefully.
3. Bed Rest
Rest helps the body heal while inflammation is active. Doctors often recommend limiting physical activity until symptoms improve.
4. Additional Support
Cases involving heart issues may require ongoing monitoring or even surgery in rare severe cases.
7.Long-Term Outlook
Many children recover fully with prompt and appropriate care, especially if the condition is diagnosed early and treated properly.
However, rheumatic heart disease — permanent damage to heart valves caused by repeated inflammation — remains a major long-term complication, especially where access to care is limited.
Children who’ve had rheumatic fever often require:
-
Long-term antibiotic prophylaxis
-
Regular heart checkups
-
Close monitoring for any new sore throats or infections
8.Prevention: How Families Can Protect Children
Preventing rheumatic fever starts with prompt treatment of strep infections. Steps parents and caregivers can take include:
✅ Treat Strep Throat Early
If your child has a sore throat, fever, or other strep symptoms, see a healthcare provider promptly. Completing the full course of prescribed antibiotics is crucial — even if your child feels better halfway through.
Good Hygiene
Teach children to:
-
Wash hands regularly with soap
-
Cover their mouth and nose when coughing or sneezing
-
Avoid sharing utensils or drinks during infections
Follow-Up Care
Children who’ve had rheumatic fever may need regular check-ups and long-term antibiotics to prevent recurrence or heart damage.
9.When to Seek Medical Help
Contact your healthcare provider if your child:
-
Has a sore throat with fever
-
Develops joint pain, rash, or unusual movements
-
Experiences chest pain or breathing issues
Early testing and antibiotic treatment for strep greatly reduce the risk of rheumatic fever.
Conclusion
Rheumatic fever is a serious, but largely preventable childhood disease. With timely treatment of strep infections, good hygiene, and proper medical follow-up, most children recover well and avoid long-term complications. However, awareness of symptoms and rapid response to strep throat remain essential for prevention.